Physical Therapy for Balance and Fall Prevention
About Fall Risk Assessment, Treatment, & Prevention Planning
According to the U.S. Congress Fall Prevention Act, falls are the leading cause of injury-related death among individuals who are over 65 years of age. In the 65+ population, the number of fall-related deaths is expected to double by 2030.
The Fall Prevention Act found that, “A national approach to reducing elder falls, which focuses on the daily life of senior citizens in residential, institutional, and community settings, is needed. The approach should include a wide range of organizations and individuals including family members, health care providers, social workers, employers, and others.”
Since 2003, the U.S. Congress has funded education and research directed toward preventing falls, enacted the Keeping Seniors Safe From Falls Act of 2006 and the Safety of Seniors Act of 2007.
As a result, Medicare now recommends that all Medicare patients receive an annual Fall Risk Assessment.
At Optimum Wellness Centers, risk of falls assessment is just one part of a complete program to help improve your balance, and reduce your risk of falling.

1 Balance & Fall Risk Assessment: Simple & Painless

A fall risk assessment is the first step for reducing fall risk and reducing the fear of falling.
A major problem confining older people to their homes is the fear of falling. In many cases, older adults are afraid to talk about this as they fear it will lead to a loss of independence.
Many seniors are afraid of falls, but even more are afraid to admit their fear.
That’s why Medicare recommends that all Medicare patients receive an annual fall risk assessment. When followed, this recommendation helps address one of the most difficult aspects of balance and dizziness problems in the elderly— the fear of losing independence. Experts suggest that the often unspoken fear of losing independence, due to admitting to having a fear of falling, can be a significant obstacle to beginning prevention planning at the earliest opportunity. Early intervention can provide the greatest chance to reduce the risk of a debilitating fall.
Comprehensive Balance & Fall Risk Assessments Include Four Types of Evaluations
Evaluation #1: Individual Risk Factors
| 1 | Muscle weakness |
|---|---|
| 2 | History of falls |
| 3 | Gait deficit |
| 4 | Balance deficit |
| 5 | Use of an assistive device |
| 6 | Visual deficit |
| 7 | Arthritis |
| 8 | Impaired ability to do activities of daily living |
| 9 | Depression |
| 10 | Cognitive impairment |
| 11 | Age > 80 years |
According to JAGS: AGS/BGS Guidelines, If you have 1 of the above risk factors, there is a 27% chance that you will fall within the next year. If you have 4 or more your chances are 78%.**
Evaluation #2: Physical Therapy Tests and Measurements
| Muscle Strength | A detailed assessment of the muscles in the legs is performed to identify key muscles that may be weak. An emphasis is placed on the muscles that are most active during standing, balance, and walking, as weakness in these muscles can lead to falls. |
|---|---|
| Balance | Balance during standing and walking is assessed both on firm (tile) and uneven (foam) surfaces. A physical therapist will also assess your gait and ability to perform pivot turns to gauge safety in the home and community. Depending on the extent of the balance deficits, your balance may also be assessed with your eyes closed. |
| Functional Limitations | A physical therapist may assess your ability to stand up from a chair, climb stairs, and traverse curbs to see where your baseline is. Overall, a physical therapist will give you exercises to help you restore and improve your individual functional limitations. |
Evaluation #3: Drug Interactions and Adverse Side Effects
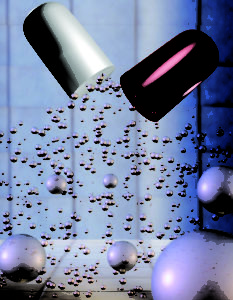 As we age, we become increasingly susceptible to the adverse side effects and interactions of medications we take. This fact is compounded by the likelihood that additional medications may be added over time to help manage newly diagnosed conditions.
As we age, we become increasingly susceptible to the adverse side effects and interactions of medications we take. This fact is compounded by the likelihood that additional medications may be added over time to help manage newly diagnosed conditions.
As part of your fall risk assessment and prevention planning program, it’s important to periodically review your symptoms and determine which ones may be due to medication. It’s extremely important to avoid mistaking any adverse symptoms you may be experiencing for normal aging when they may be more directly related to adverse drug side effects and interactions.
Please do not stop taking any prescribed medication without consulting with your doctor. Many medications must be gradually weaned to avoid serious complications.
Evaluation #4: Home Safety
When you are prone to falling, your home can either support you or become a reason for your falls. The following is a list of common things that make a difference in lowering the risk of falls due to home hazards. Look around your home environment and think about your home is helping you avoid falling. You may need to change things to make it less likely that you will fall.
- Avoidable Trips – Remove all clutter, electrical cords, low furniture, area rugs, or other items that impede pathways.
- Handholds – Make sure sturdy handholds are placed room to room in case you feel unsteady or lose your balance.
- Lighting – Make sure lighting is adequate, especially in the bathroom, kitchen, hallway, and bedroom.
- Footwear – Avoid loose fitting slippers and wear comfortable shoes.
- Bath & Toilet – If you have difficulty getting into the bath/shower, or up and down from the toilet, consider assistive fixtures and equipment recommended by your physical therapist or medical supplier.
- Stairs – Consider adding additional handrails, or modifying a room configuration to improve safety in the home. Limiting the use of certain living levels may be necessary.
- Reach – Make sure all household items are accessible without extending, overreaching, or standing on tip-toes.
- Outside – In the places you walk outside, identify and fix areas with uneven or slippery surfaces, cracks, or other potential hazards.
- Help – Make sure you have a way to get help quickly should you fall or are unable to get up.
2 Balance Treatment & Fall Risk Prevention
Your Physical Therapist Will Summarize Your Evaluation Results and Formulate a Treatment Plan That Is Designed Specifically For You.
- If muscle weakness or tightness is found, then you will begin a series of exercises that will strengthen and stretch the muscles.
- Balance deficits can be treated through a series of exercises designed to specifically target and improve the body’s balance systems. These exercises have been proven in clinical studies to improve balance regardless of the person’s age.
- As strength and balance improve, we can tie it all together by working on any functional skill that you are having difficulty with.
- How long will it take to see improvement? Most patients experience improvements within 4-6 visits, attending two to three times weekly.
- Will Medicare pay for treatment? Physical therapy treatment for balance problems including muscle weakness, difficulty walking, dizziness, and a history of falls are all covered by Medicare, as well as most other insurance plans, within the limitations of coverage guidelines.
| Balance Retraining | |
|---|---|
| Static/Dynamic Balance Retraining | |
| Habituation/Adaptation | |
| Strengthening/Aerobics | |
| Education/Customized Home Program | |
| Gait Training | |
| Functional Retraining (curbs, stairs, uneven surfaces) | |
| Neurological Evaluation & Treatment | |
| Neuromuscular facilitation exercises | |
| Assessment of abnormal muscle tone | |
| Assess for an assistive device | |
| Annual Fall Risk Assessment | |
| Therapeutic Exercise | |
| Progressive resistive strengthening | |
| Muscle stretching |

