Physical Therapy for Muscle and Joint Pain
According to the Center for Disease Control, nearly 20 million US adults live with severe joint pain…
…In fact, the number one CDC recommendation for muscle and joint pain is to get physically active. A popular saying in physical therapy is “motion is lotion.” Any increase in exercise needs to be done safely, especially when there is an underlying condition causing your muscle and joint pain.
Your Optimum Wellness Centers physical therapist assures you receive a medically supervised evidence-based plan of care.
Can your muscle and joint pain resolve more quickly and completely with physical therapy? Take this 5-question self-assessment to find out:
- Do you have muscle or joint pain that has not resolved for more than two weeks?
- Do you avoid using an arm or leg due to pain?
- Have you recently engaged in new activities or increased your exercise and noticed soreness that isn’t going away?
- Are you still struggling with pain and stiffness after an injury or surgical procedure?
- Do you take pain medication for daily aches and pains?
If you answered YES to any of these questions, a customized physical therapy program may be the answer you have been looking for.
1 Assessment - Muscle and Joint Pain
Quick Facts & Assessment Table
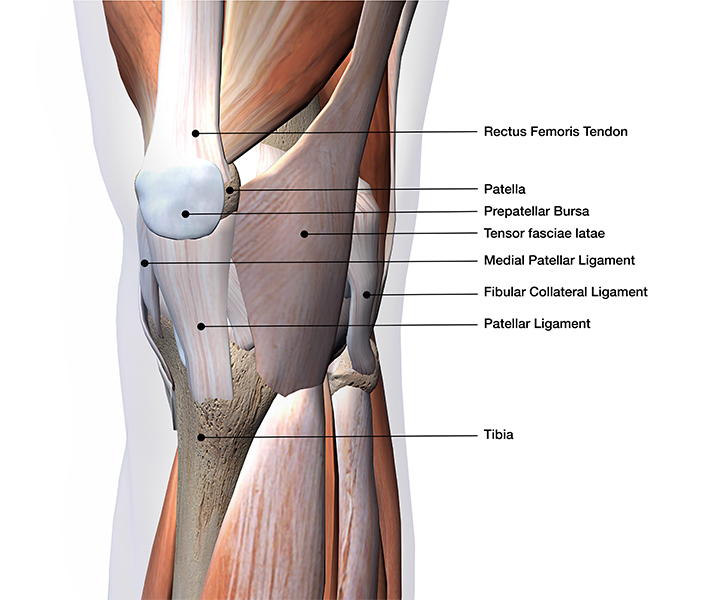
What’s the difference between a muscle, tendon, and ligament?
- A muscle is made up of groups of contractile fibers that have the ability to stretch.
- A tendon connects muscle to bone. It is less flexible and contractile than a muscle. A tendon is made up of more dense, fibrous tissue.
- A ligament connects bone to bone. It is the least flexible of the three types of tissues.
What’s the difference between a sprain and a strain?
- A sprain and strain are the same thing- an overstretching or tearing of tissue. The terms are applied to describe the type of tissue injured. A muscle is strained, and a ligament is sprained.
- There are different types of sprains and strains, with different symptoms and healing times, as described in the table below:
Assessment Table
Grade I
 Stretching, small tears |
Grade II
 Larger, but incomplete tear |
Grade III
 Complete tear |
|
|---|---|---|---|
| What is it? | Muscle/ligament fiber separation. This occurs as the fibers become over-stretched (<5%) | Other names: partial thickness or incomplete tear. The muscle/ligament fibers are torn but are still connected. In a mild strain/sprain, the area may feel slightly stiff, but still flexible enough for use. In a more severe strain/sprain, there is pain and very limited movement. | The muscle/ligament fibers tear- full thickness/complete tear: Muscle/ligament fibers completely separate away from each other and are no longer connected. |
| Signs and Symptoms |
|
|
|
| Healing Time | May take a few weeks to heal. | A mild to moderate sprain/strain will usually heal within a few weeks to a few months. | More severe strains may take months to a year to heal. |
What is tendonitis/tendonopathy?
Tendonitis is an acute inflammation or irritation of a tendon (less than 3 months). Tendinosis/tendinopathy is a CHRONIC inflammation of a tendon (greater than 3 months).
How do Sprains/Strains/Tendonitis occur?
| Strains | Tendonitis | Sprains |
|---|---|---|
|
|
|
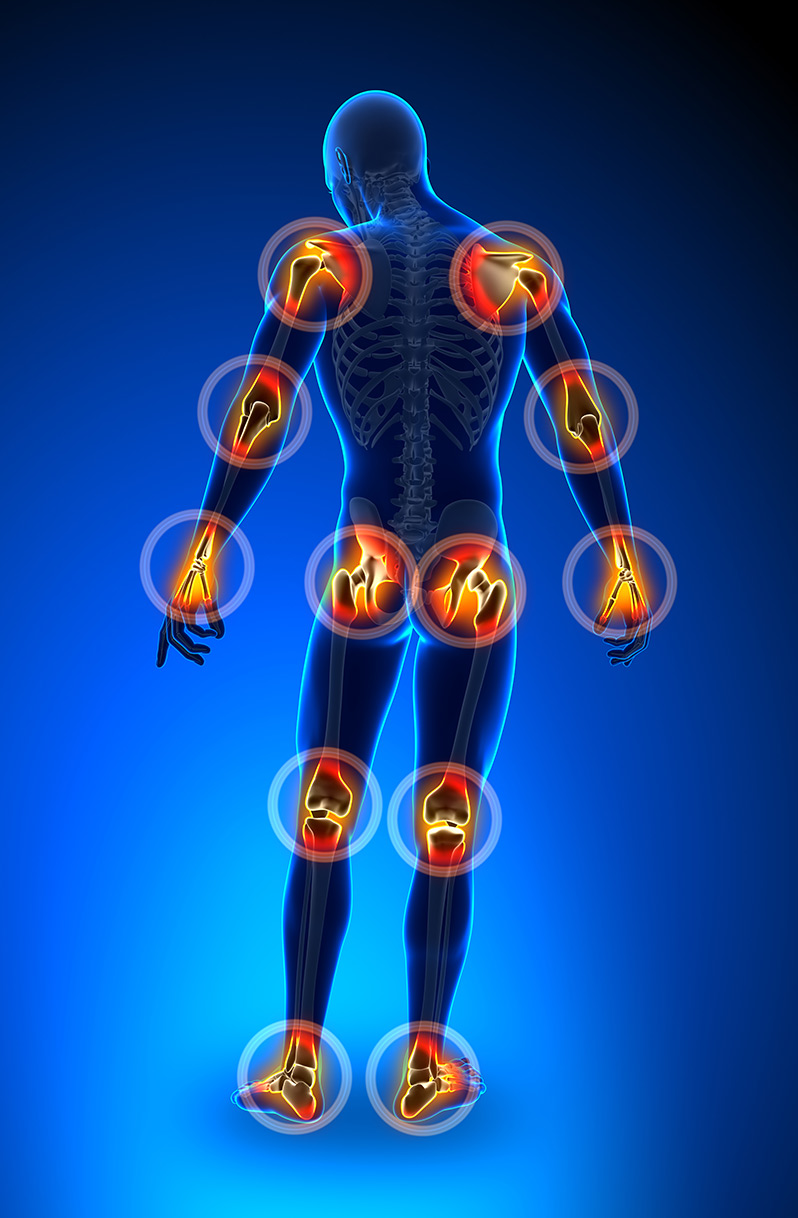
What is joint pain?
- Joint pain refers to discomfort, aches, and soreness in any of the body’s joints.
- Many different conditions can lead to painful joints, including: osteoarthritis, rheumatoid arthritis, bursitis, gout, strains, sprains, and other injuries.
- Joint pain is extremely common. Knee pain is the most common complaint, followed by shoulder and hip pain.
- Signs and Symptoms:
- The area around the joint is swollen, red, tender, or warm to the touch.
- Pain persists for three days or more.
- Pain that increases with movement.
How does joint pain occur?
- Can occur from natural wear and tear over time.
- Can be related to a fall or other form of trauma.
- Can be related to another disease/condition.
When should you seek physical therapy?
- When you have pain that does not subside within a week.
- Loss of range of motion/ ability to perform tasks/activities.
- Increased weakness/stiffness limiting ability to perform functional activities such as bathing/washing, dressing, reaching into a cabinet, picking up objects from the floor, etc.

What should you expect in physical therapy?
To begin, your Optimum Wellness Centers physical therapist will determine if the joint is affected, or if the muscle/ligament is partially or completely torn by performing special orthopedic tests. In addition, a doctor may prescribe other tests such as a CT-scan, MRI, and X-ray. Based on the results of your exam and your personal goals, an individual plan will be established to help you get back to your daily activities.
2 Treatment & Condition Management at Home - Muscle and Joint Pain
A physical therapist may give you a Home Exercise Plan (HEP) to help start and continue your recovery at home through the use of stretches and/or exercises.
- Rest
- A physical therapist will determine if there are certain tasks/activities that you should not be doing while your body heals. You want to rest the area, and avoid movement that increases pain and may lead to further injury.
- Don’t rest for too long, as it can lead to weakness and stiffness.
- Ice
- For acute injuries (< 3 months)
- Reduces inflammation/edema
- Reduces pain
- Avoid application of ice direction to the skin. Limit icing time to 15-20 minutes to reduce the potential for frostbite.
- Heat increases inflammation and edema, which can increase pain, and decrease ability to move.
- Heat
- For chronic injuries (>3 months)
- Increases blood flow/circulation
- Decreases muscle guarding and stiffness
- Increases tissue flexibility
- Avoid application of heat direction to the skin. Limit time to 15-20 minutes to reduce the potential for burns.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)***
- Reduces inflammation/edema
- Reduces pain
- ***Check with your doctor to see if appropriate, and if there are any conflicts with other medications you may be taking.
- Compression
- Do not wrap too tightly.
- A compression wrap or sleeve can help protect and support the injured area.
- Prolonged use can lead to weakness.
3 Progress & Prevent - Muscle and Joint Pain
- Help avoid injury by stretching/warming-up/cooling-down before and after activity. Take time to maximize the range of motion of your joints. This can help to minimize repetitive trauma on tight tissues.
- Watch your form when lifting, especially when performing repetitive sport movements or job-related activities. Improper technique can overload the tissue and lead to injury.
- Avoid activities that place excessive stress on the tissue, especially for prolonged periods.
- Change up your exercise. Cross-training can help you mix up an impact-loading exercise, and reduce stress to your tissues.
- Make an effort to stay in shape.

